
Kris Kowdley of Virginia Mason Medical Center. Photo by Liz Highleyman/ hivandhepatitis.com.
A number of important studies were presented
concerning the safety and effectiveness of new anti-hepatitis C (HCV) drugs
used in combination without interferon.
The results of several studies were highly
encouraging.
Current HCV therapy is based on pegylated interferon and ribavirin. These drugs don't always work and can cause
unpleasant side-effects.
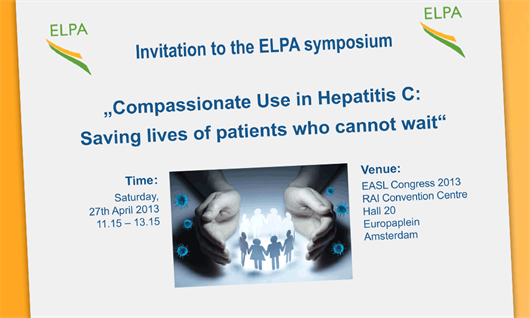
But results presented to the Amsterdam conference
showed that an interferon-free combination of drugs that work directly against
HCV can achieve a 90% cure rate. The
study involved people with genotype 1 infection.
Other research showed that a two-drug combination of direct-acting drugs
can achieve high rates of sustained virological response (SVR, considered a
cure) in people with the easier-to-treat genotype-2 infection.
Another combination of three drugs being developed by Bristol-Myers Squibb cured over
90% of patients with genotype 1 infection after 12 weeks of treatment.
Most of these interferon-free combinations
will need to be studied in larger trials before they are licensed for use.
Nevertheless, it seems likely that HCV treatment consisting entirely of
direct-acting agents will be a reality within a few years.
Until then, pegylated interferon will remain
a mainstay of therapy.






Connect with infohep on Facebook: Keep up to date with all the latest news and developments.
Follow infohep on Twitter for links to news stories and updates from infohep.org. Follow us at www.twitter.com/infohep.
Follow all the infohep news by subscribing to our RSS feeds.